2014 Research Report
Dear OCI supporters,
The past year was scientifically the most productive year for the Ovarian Cancer Institute lab since my arrival at Georgia Tech. We published 13 major research papers in 2014 (listed below) and we were awarded a new patent in 2014 (“MIR-200 family induces mesenchymal-to-epithelial transition”; issue date: 11/25/2014).
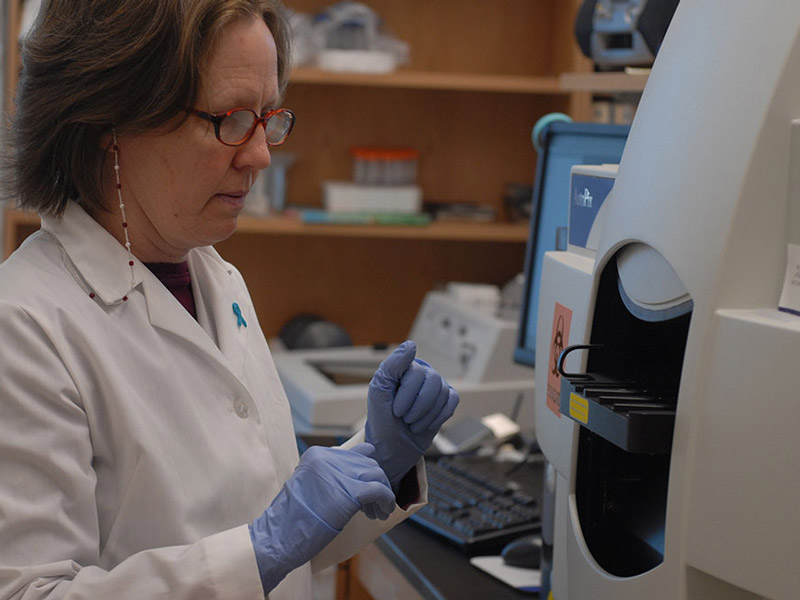
On the diagnostic side, much of our focus remains on the use of MASS SPEC-based metabolic profiling to identify metabolic biomarkers of ovarian cancer (OC) in the blood. As you may recall, several years ago we published a paper showing that metabolic profiling can distinguish blood sera collected from OC patients (relative to normal healthy women) with extremely high accuracy (Zhou M, Guan W, Walker LD, Mezencev R, Benigno BB, Gray A, Fernandez FM and McDonald JF. 2010. Rapid Mass Spectrometric Metabolic Profiling of Blood Sera detects Ovarian Cancer with High Accuracy. Cancer Epidemiology, Biomarkers and Prevention Sep; 19(9): 2262-71). While the findings were well received, the drawbacks were that this study was carried out using serum samples mostly from stage III OC patients (since the disease is asymptomatic in early stages, blood samples from early staged patients are very rare) and a molecular diagnostic for late stage OC is of little clinical significance. We have now improved our assay and have applied it to prostate cancer serum samples and to nearly 100 early staged ovarian cancer samples. The prostate study has recently been published (Zang et al 2014-see below), and the ovarian cancer results (see figure below) are currently being written-up and we anticipate publication in early 2015.
We are excited about our new findings because not only is the test highly accurate but we have been able to limit the number of diagnostic metabolites to 20 molecules for which we have specific identities. We think this study will have a significant impact on the ovarian cancer community when it is published early in 2015. We are currently negotiating with a number of private and commercial entities to validate our assay prospectively in 500-1000 women considered to be at high risk for OC (i.e. women with previous family history of OC, women who have tested positive for BRAC mutations, women of Ashkenazi Jewish ancestry, etc.). The ovarian cancer diagnostic studies have and continue to be possible through your support.
Another major focus of our lab is on the development of novel RNA-based OC therapeutics. While current cancer drugs act on the protein level, we believe this approach will be seen as inadequate as we move into the era of genomic profiling and personalized, targeted gene therapy. The reason for this is that genomic profiling of tumors has the potential to identify specific genes that are abnormally expressed in individualized tumors (“Personalized Cancer Medicine”). However, it is estimated that only 10% of abnormally expressed genes can be inhibited on the protein level (most proteins are not responsive to small inhibitory molecules). In contrast, all genes can, in principle, be inhibited on the RNA level with small regulatory RNAs (siRNAs & miRNAs). Our laboratory continues to be a leader in the development of small regulatory RNAs for the treatment of OC and the majority of our publications in 2014 are devoted to this topic.
We have been specifically focusing on inhibitory RNAs that can block cancer metastasis because this is generally considered to be the most lethal component of all cancers. Our recent patent is based upon our discovery that ectopic expression of a specific class of small regulatory RNAs (the MiR-200 family of microRNAs) can effectively block/reverse the development of metastatic OC cells. While the biological potential of miRNAs as an effective cancer therapeutic is becoming more widely appreciated, a major barrier to clinical application is the inability to target delivery of these inhibitory molecules to cancer cells. In collaboration with a number of our colleagues at Georgia Tech, we have and continue to work hard on this problem. Our initial efforts with Dr. Andrew Lyon’s lab in the School of Chemistry to develop nanohydrogels as delivery vehicles continues to be highly promising and over the past 3 years has led to a number of publications, the award of a small NIH pilot grant as well as a patent issued two years ago. Efforts over the next year will be to demonstrate biological efficacy of nanohydrogel delivery of miR-200 family RNAs in a mouse model of OC.
As a backup to these studies, we continue to collaborate with other scientist/engineers at Georgia Tech to develop potentially even more efficient delivery vehicles. We are currently most excited with studies recently initiated with Dr. M.G. Finn in the School of Chemistry to develop viral particles for the delivery of therapeutic RNAs. What I consider most interesting is the fact that bacterial cells are being engineered to not only manufacture these particles, but to package them with our therapeutic RNAs all in vivo thereby by-passing the extensive efforts/costs associated with the synthesis and packaging of delivery particles in the lab. These exploratory studies are made possible by your financial support.
A final new area of research in our lab is highly computational in nature and is centered on the development of algorithms to predict optimal drug therapy from genomic profiles of individual patient tumors. This is a hot area of investigation in the field of cancer biology and a number of commercial entities have already been established purporting to provide patients with such predictions based on tumor genomic profiles (e.g., Foundation Medicine, Inc., Cares, Inc., Precision Diagnostics, Inc. etc.). The problem is that the basis of current predictions is based on our extremely limited understanding of the cause of most cancers. In those few cancers where this causal-based understanding is reasonably well understood (e.g., over-expression of tyrosine kinase in various blood cancers), optimal drug predictions are reasonably good (e.g., tyrosine inhibitors such as Gleevec work quite well). However, in most cases, genomic profiling based predictions of optimal drug therapies are extremely inaccurate. Our strategy is to take a non-causal based approach to drug predictions. Our approach is not unlike the approach taken by Netflix in predicting movies clients are likely to enjoy based upon personal profiles. In our case, we are collaborating with computer scientists at Georgia Tech to develop machine based (support vector machines) learning algorithms that input genomic profiles and drug response profiles of thousands of cancer samples and generate predictive models to predict one from the other. Thus far, our models have proven to be extremely accurate (80-100%) in predicting the drug responsiveness of over ten different types of human cancer cells based on DNA sequence and gene expression profiles. We will be expanding these studies to human patient samples over the next year. These pilot studies are made possible by your financial support.
I have always felt that the best way to acknowledge thanks for financial support is to show that it has been used responsibly and effectively. I hope you will agree that we have used your generous financial support creatively and productively over the past year and that progress continues to look good for the future. Thank you sincerely for all of your help.
John McDonald
Chief Scientific Officer

