What Is Personalized Cancer Medicine?
We’re all different. Why? Because (with the exception of identical twins) the blueprint that determined what we are (otherwise known as our DNA or our genome), is different between each one of us. Indeed because we are all different, we would consider it silly to think that we are all going to enjoy the same kind of food or wear the same clothes, or enjoy the same kind of music.
We now know that all cancers are different as well–and for the same reasons. Even cancers of the same type, like ovarian cancers, can be genetically quite different from one another. Thus, why should we expect that all ovarian cancers will respond equally well to the same therapies? In fact, physicians have known for a long time that not all patients with the same type of cancer respond identically to the same chemotherapies. For example, some ovarian cancer patients respond very well to standard first line therapies (e.g., carboplatin/taxol) but some do not.
Personalized cancer medicine is the idea of analyzing the genome of each patient’s tumor individually and, based on this information, designing chemotherapies customized to specifically target the gene or geness identified to be malfunctioning in each individual patient. In recent years several companies have been established (e.g., Foundation Medicine in Massachusetts) that will analyze the DNA profile of individual tumor patients and provide physicians with recommended therapeutic options. Although this is every cancer physician’s dream scenario, the problem is that most of the recommendations currently being made simply don’t work.
The Big Challenge-Going From Genome Profiles to Customized Targeted Gene Therapies
Before talking about why most genomic based drug predictions currently don’t work, let’s consider one of the few examples where it does-the treatment of chronic myelogenous leukemia (CML) with the receptor tyrosine kinase (TK) inhibitor Gleevec (imatinib). This drug is known to specifically inhibit a specific type of mutation that can be readily identified in genomic profiles of CML patients. The problem is that most cancers, including ovarian cancers, are not associated with this particular class of mutation. From what is currently known, it appears that most solid tumors, like ovarian cancers, are genetically more complicated than blood cancers. Indeed, it appears that there are many molecular paths to the development of ovarian and other solid tumors and we are still years away from specifically identifying each of these alternative pathways. Thus, for the vast majority of cancers where our understanding of the molecular basis of the disease remains incomplete, we are most likely years away from being able to generate knowledge-based predictions of optimal chemotherapies.
Unique Approaches Being Taken at the OCI Laboratory.
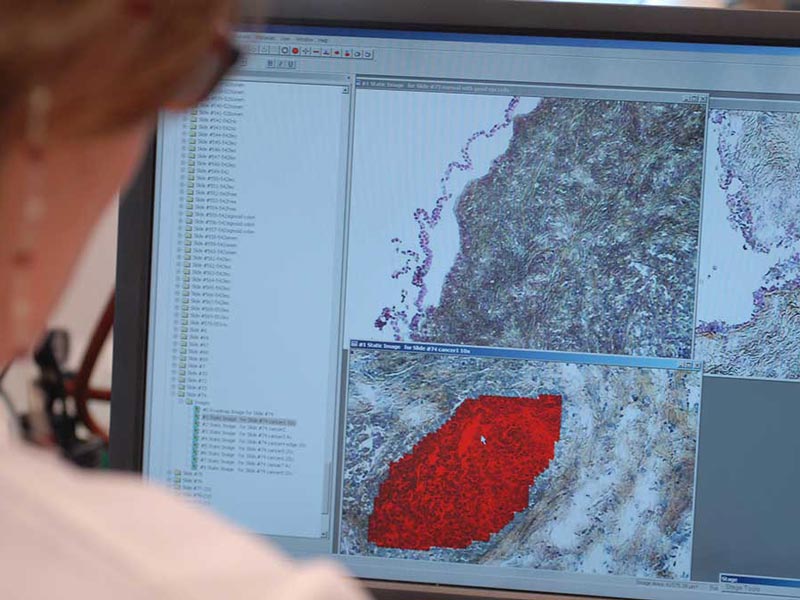
Like many other labs, we’re working hard to understand the molecular basis of ovarian cancer on an individual patient level but unlike other labs, we are taking unconventional approaches that leverage the unique strengths in the computational and technical sciences that exist at Georgia Tech.
With regard to the challenge of predicting optimal drug therapies, we are pioneering an approach that utilizes sophisticated computer “learning algorithms” that connect genomic profiles with optimal drug responses without the necessity of understanding the underlying causal processes involved. This approach is not unlike the approach taken by NETFLIX in predicting what movies you are likely to enjoy in the future based on your past choices and the choices of others with similar personal profiles.
We have been testing our approach using a set of over 500 human cancer cell lines that have been genomically profiled (DNA and RNA sequence etc.) and also tested for responsiveness to over 1000 existing and experimental drugs at the National Institutes of Health (NIH) laboratories. We have developed algorithms that can accurately (up to 100% accuracy for ovarian cancer cells) predict the positive response of cancer cells to specific drugs based on their genomic profiles. Over the next year, we will be testing these predictive algorithms using ovarian cancer patient samples. We are extremely optimistic that this novel approach to optimize personalized drug predictions will translate into significant improvements in the treatment of ovarian cancer in the near future.
John McDonald
OCI Chief Scientific Officer


